Hi!
Happy November. I am ready for it!
So, I have been meaning to write about the correlation between bone and stone disease for a while now and figured today was the day.
Dr Coe, my mentor, has always said, “Wherever you see a stone clinic, a bone clinic is close by.”
When I review patients’ 24-hour urine collection reports, I often tell them to ask their doctor to order a bone scan to rule out osteoporosis. This this goes for men as well, who are often overlooked when ordering scans to check bone health.
A common culprit of kidney stones is high urine calcium, which may be the reason for osteoporosis. I can’t tell you how many patients write me after their urine consult and say, “Jill, you were right, I have some bone loss.”
Kidney stones and osteoporosis may seem like separate health issues, but they share important connections around how the body handles calcium, vitamin D, and even the balance of acids and bases in our system. Understanding these links can help you make lifestyle changes that protect both your kidneys and bones.
Calcium’s Role in Both Conditions
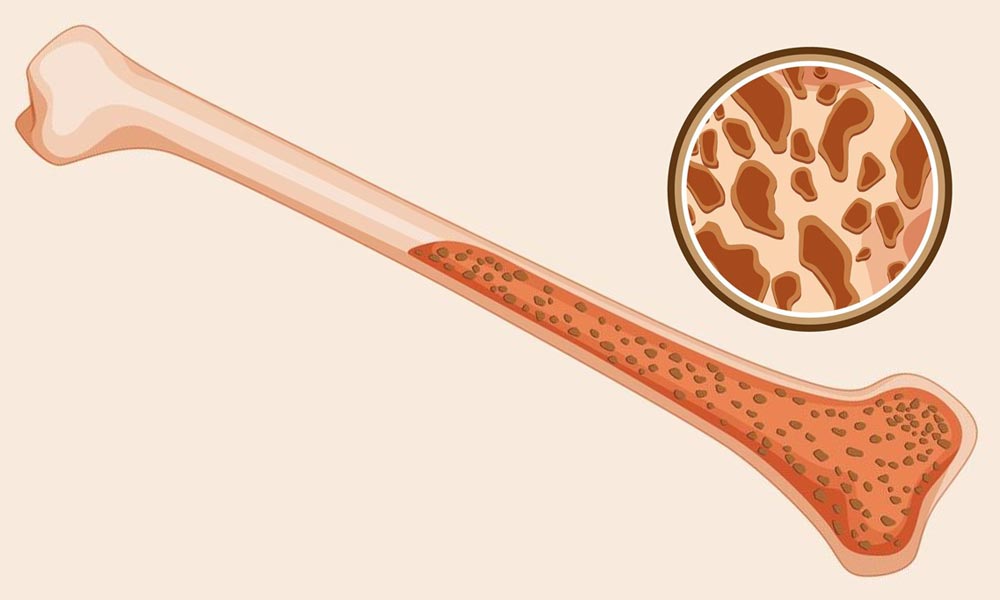
Calcium is essential for building strong bones. When it isn’t managed correctly in the body, however, it can contribute to both osteoporosis and kidney stones. In osteoporosis, bones lose calcium over time, becoming weak and brittle. In kidney stones, calcium can collect in the urine, crystallize, and form stones.
One common misconception is that reducing calcium intake will prevent kidney stones. Not eating enough calcium can make you more likely to develop stones and increase your risk for osteoporosis. When dietary calcium is low, the body pulls calcium from bones, weakening them. Additionally, without enough calcium, oxalate from foods is more likely to bind in the urine and form stones rather than being excreted normally.
Hormonal and Metabolic Factors
The body’s parathyroid glands play a significant role in regulating calcium. When calcium levels in the blood drop, these glands release a hormone that pulls calcium from bones, which weakens them over time. This process is accelerated in conditions like primary hyperparathyroidism, where high levels of this hormone cause a constant release of calcium from bones, increasing both bone loss and the risk of kidney stones.
Vitamin D is essential for calcium absorption from the diet. Low vitamin D levels make the body pull more calcium from bones, weakening them. However, too much vitamin D, particularly from supplements, can cause an overload of calcium, contributing to stone formation in susceptible individuals. The right balance of vitamin D is crucial for maintaining bone strength without increasing kidney stone risk.
Acid-Base Balance and Bone Health
Diets high in animal proteins and sodium can create an acidic environment in the body. This acidity promotes specific kidney stones (like uric acid stones and calcium oxalate stones) and encourages calcium release from bones as a natural buffer to neutralize acids. Over time, this process can accelerate bone loss, making it more challenging to maintain strong bones. Including more alkaline foods—such as fruits, vegetables, and legumes—can help offset acidity and support both kidney and bone health. Of course, mind the oxalate in your chosen foods and eat within average portion size!
Gut Health and Calcium Absorption
Digestive health also affects calcium absorption. Conditions like inflammatory bowel disease (IBD) or surgeries altering the digestive tract (bariatric surgeries) can interfere with how well calcium is absorbed. Poor calcium absorption weakens bones and leads to higher amounts of unabsorbed calcium in the gut, which binds with oxalate and increases the risk of stone formation.
Lifestyle Changes Can Help
Adopting a few fundamental lifestyle changes can support bone density and reduce the risk of kidney stones (hint follow the KSD):
- Stay Hydrated: Drinking enough water dilutes urine, reduces stone risk, and supports overall metabolic health.
- Pairing Calcium with Oxalate: Eating/drinking calcium with meals (instead of in isolation) can help prevent oxalate from binding in the urine, reducing stone risk while supporting bone health. Here is an article on how to get enough calcium. And for my non dairy folks, read this.
- Limit Sodium and Processed Foods: Excess sodium causes more calcium to be excreted in the urine, increasing stone formation and contributing to bone loss.
- Limit Added Sugars: Too much sodium, like too much-added sugar, will increase urine calcium.
- Limit Meat Protein: Acts the same as the above entries. Too much meat pulls calcium from the bone, making your urine more acidic.
- Watch Oxalate Intake: Certain high-oxalate foods (like spinach, beets, and higher oxalate nuts) can contribute to kidney stones, but pairing them with calcium-rich foods can help bind oxalate in the gut rather than the urine. Get your oxalate list here.
- Get Balanced Vitamin D: Ensuring you get enough, but not excessive, vitamin D helps maintain calcium absorption without increasing the risk of stones. Knowing how much will require a blood test to see where your d level is right now. If you do go on a supplement, recheck your vitamin D blood level in several weeks (it takes a bit for vitamin D to be absorbed) to see if your level is better, and then go on a maintenance dose to keep it there. Your doctor must order the blood test and help you with the correct vitamin D dosage.
Notice that all of the above is in the Kidney Stone Diet®. It will help lower your risk of stones, bone disease, and many other disease states.
Special Considerations for Women
Women, especially after menopause, face a higher risk for osteoporosis and kidney stones. Lower estrogen levels can lead to faster bone loss, and specific hormone changes also impact calcium excretion. At this stage, balancing calcium and vitamin D, reducing sodium and sugar intake, and adding weight-bearing exercise becomes even more crucial to supporting bone health and preventing stones. This is why I always get my strength training in. I implore you to consider incorporating strength training into your fitness goals.
Bottom Line
Kidney stones and osteoporosis are deeply connected through how the body regulates calcium, vitamin D, and our acid-base balance. By making small, targeted lifestyle changes, you can help protect your bones and kidneys, reducing the risk of these common but challenging conditions.
Follow the Kidney Stone Diet to get you started on the right path!
Your friend and advocate,
Jill











Leave a Reply